December 8, 2020
Assessing the age specificity of infection fatality rates for COVID-19: systematic review, meta-analysis, and public policy implications
Before we begin let us define the difference between case fatality rate (CFR) and infection fatality rate (IFR).
CFR is the ratio of the number of deaths divided by the number of confirmed (preferably by nucleic acid testing) cases of disease.
IFR is the ratio of deaths divided by the number of actual infections with SARS-CoV-2.
And let’s define:
Seroprevalence is the level of a pathogen in a population, as measured in blood serum.
https://link.springer.com/article/10.1007/s10654-020-00698-1
While the NYC data indicate a population IFR of about 1%, seroprevalence estimates from other locations have yielded a wide array of population IFR estimates, ranging from about 0.6% in Geneva to levels exceeding 2% in northern Italy. Such estimates have fueled intense controversy about the severity of COVID-19 and the appropriate design of public health measures to contain it, which in turn hinges on whether the hazards of this disease are mostly limited to the elderly and infirm. Indeed, a recent meta-analysis noted the high degree of heterogeneity across aggregate estimates of IFR and concluded that research on age-stratified IFR is “urgently needed to inform policymaking.”
.
Editor:
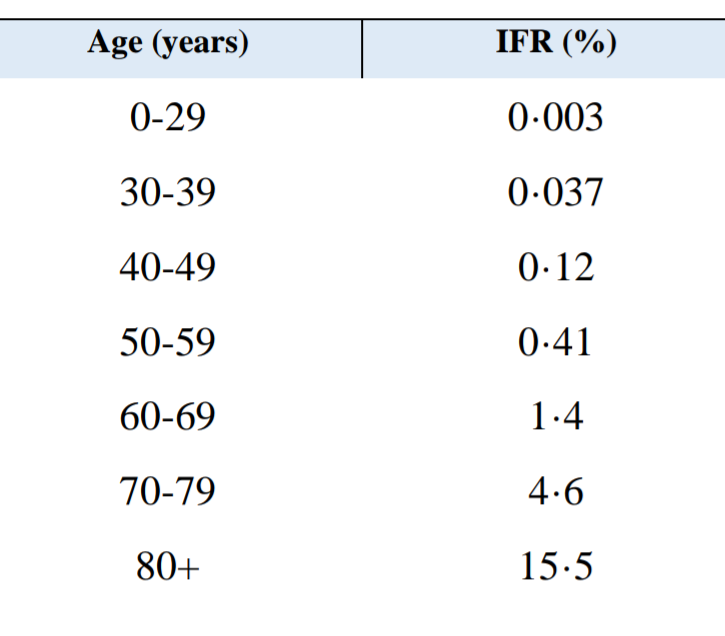
Contrapositive Infection Survival Rate by Age:
0-29 years: 99.997%
30-39 years: 99.963%
40-49 years: 99.88%
50-59 years: 99.59%
60-69 years: 98.6%
70-79 years: 95.4%
80+ years: 84.5%%
.
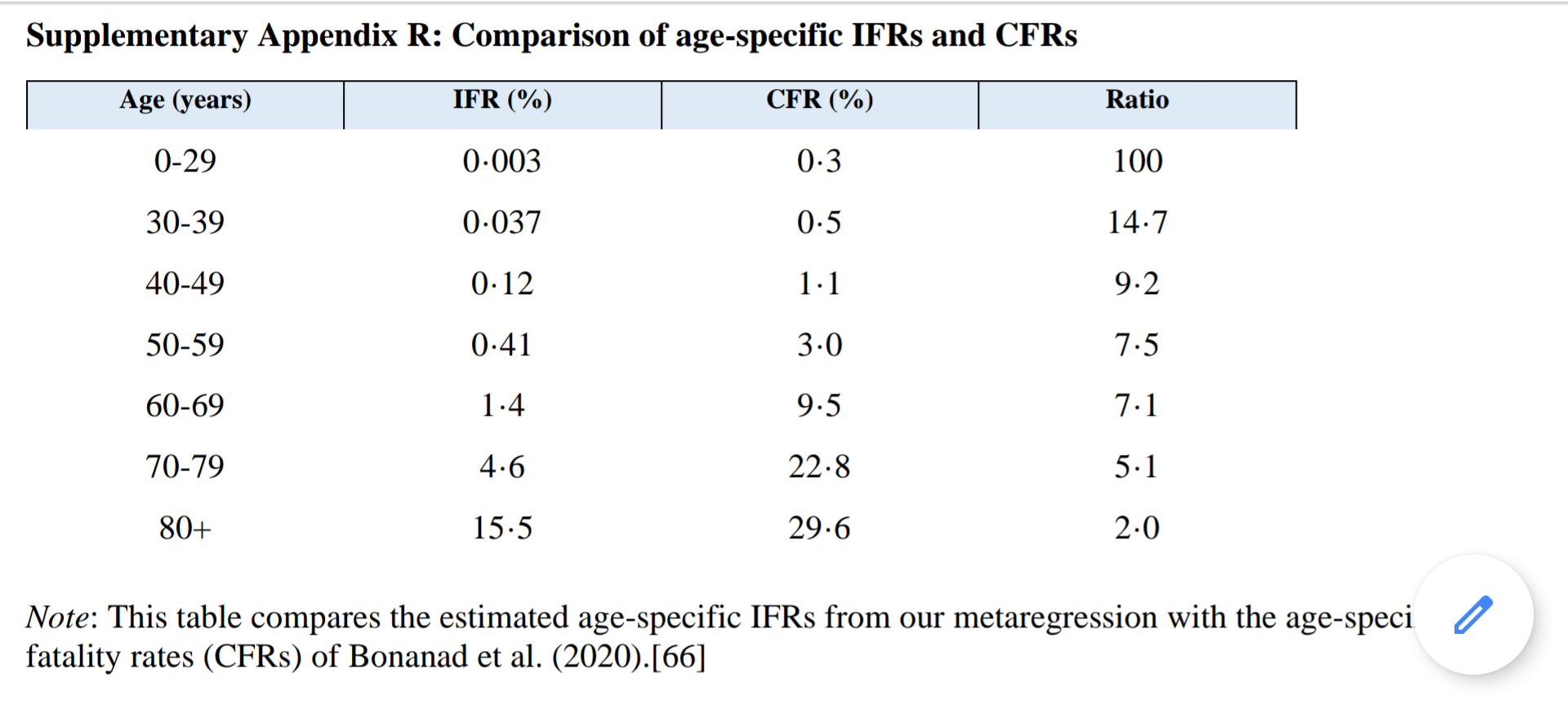
The exponential pattern of our age-specific IFR estimates is qualitatively similar to that of case fatality rates (CFRs). However, the relative magnitudes are systematically different, reflecting the extent to which asymptomatic or mildly symptomatic cases are much more common in younger adults than in middle-aged and older adults. For example, the ratio of CFR to IFR is about 15:1 for ages 30–49, about 7:1 for ages 50–69, and about 5:1 for ages 70–79 years
.
Our analysis finds a exponential relationship between age and IFR for COVID-19. The estimated age-specific IFR is very low for children and younger adults (e.g., 0.002% at age 10 and 0.01% at age 25) but increases progressively to 0.4% at age 55, 1.4% at age 65, 4.6% at age 75, and 15% at age 85.
.
.
This paper reports on a systematic review and meta-analysis of age-specific IFRs for COVID-19. We specifically consider the hypothesis that the observed variation in IFR across locations may primarily reflect the age specificity of COVID-19 infections and fatalities. Based on these findings, we are able to assess and contextualize the severity of COVID-19 and examine how age-specific prevalence affects the population IFR and the total incidence of fatalities.
.
Likewise, our metaregression does not include measures of comorbidities such as diabetes or obesity.
.
Another limitation of our meta-analysis is that we have focused exclusively on assessing IFRs in advanced economies to facilitate comparability regarding health care provision and reporting of fatalities. Nonetheless, it is absolutely clear that the COVID-19 pandemic has had devastating consequences for lower-income and developing countries. For example, as of late October 2020, the reported COVID-19 death counts were nearly 160 thousand in Brazil, 120 thousand in India, and 90 thousand in Mexico. And in many countries, measures of excess mortality are much higher than official tabulations of COVID-19 fatalities.
.
Consequently, analysis of prevalence and IFR is urgently needed to provide guidance to public health officials in developing countries. However, the core findings of our meta-analysis may well be relevant even in those contexts. For example, recent prevalence studies of Manaus, Brazil found that about 66% of the population was infected with the SARS-CoV-2 virus between March and August 2020. As of October, Manaus (a city with 1.8 million inhabitants) had 2853 confirmed COVID-19 deaths. That outcome is remarkably consistent with our analysis, because nearly 90% of Manaus residents are under 50 years of age. Indeed, using the age structure of the Manaus population and assuming uniform prevalence of infections across age groups, our metaregression predicts a population IFR of 0.22% that is practically indistinguishable from the observed outcome of 0.2%. Thus, our analysis provides a coherent explanation why Manaus was much less severely impacted by the pandemic compared to other locations with larger numbers of middle-aged and older adults.
.
One key implication of our findings is that the incidence of fatalities from a COVID-19 outbreak depends crucially on the age groups that are infected, which in turn reflects the age structure of that population and the extent to which public health measures limit the incidence of infections among vulnerable age groups.
.
Editor:
Morbidity rate is defined as the measure of
illness, rather than mortality. Covid-19 can cause extended illness in people with advanced age, excess weight and pre-existing medical conditions. It is important for this reason (morbidity, as well as mortality) to avoid exposure to the virus.